http://dx.doi.org/10.24016/2022.v8.260
ORIGINAL ARTICLE
An explanatory model of suicidal ideation based on
family functionality and mental health problems: A cross-sectional study of
medical students
Un modelo explicativo de la ideación suicida basado en
la funcionalidad familiar y los problemas de salud mental: Un estudio
transversal de estudiantes de medicina
Leslie Aguilar-Sigueñas 1*, David
Villarreal-Zegarra 2
1 Universidad César Vallejo, Escuela de Medicina, Piura, Peru.
2 Instituto Peruano de Orientación Psicológica, Lima, Peru.
* Correspondence: Leslie Aguilar-Sigueñas. E-mail: leslieemilyaguilar@gmail.com.
Received: February 23, 2022. | Revised: November 01,
2022. | Accepted: December 15, 2022. | Published Online: December
15, 2022.
CITE IT AS:
Aguilar-Sigueñas, L., &
Villarreal-Zegarra, D. (2022). An explanatory model of suicidal ideation based
on family functionality and mental health problems: A cross-sectional study of
medical students. Interacciones, 8,
e260. http://dx.doi.org/10.24016/2022.v8.260
ABSTRACT
Background: One of the mental health problems with the greatest
impact on people’s lives is suicidal behavior, a largely preventable public
health problem that accounts for almost half of all violent deaths. The
aim of the study is to propose a model that can explain and predict suicidal
ideation based on mental health problems (stress-anxiety-depression) and family
functionality (cohesion, flexibility, and cohesion). Methods: Our study
is cross-sectional. The population consisted of medical students from all over
Peru. Non-probability sampling was used. We used Family Cohesion and
Adaptability Evaluation Scale (FACES-III), Family Communication Scale, Family
Satisfaction Scale, Depression Anxiety and Stress Scales (DASS-21), and the
Scale for Suicide Ideation – Worst (SSI-W). Results: A total of 480
participants were included. The prevalence of suicidal ideation was 39%.
Poisson regression analysis adjusted identified that people with anxiety
symptoms were more than four times more likely to have suicidal ideation
(PR=4.89; 95% CI:1.90-12.64). Also, people with moderate to high levels of
family communication were much less likely to have suicidal ideation (PR= 0.07;
95% CI: 0.01-0.41), making it a protective factor. The proposed model presented
optimal goodness-of-fit indices (CFI=0.974; TLI=0.974; SRMR=0.055;
RMSEA=0.062). In addition, the proposed model can explain the presence of
suicidal ideation in 88.3% (R2=0.883). Conclusions: Our model
can explain 88.3% of suicidal behavior based on family relationships and mental
health problems in medical students. In addition, the variables that alone were
most associated with suicidal behavior were anxious symptoms and family
communication as risk factors and protective factors, respectively.
Keywords: suicidal ideation, depression, anxiety, family,
stress.
RESUMEN
Antecedentes: Uno de
los problemas de salud mental mayor impacto en la vida de las personas, es la
conducta suicida, que constituye un problema de salud pública en gran medida
prevenible, siendo responsable de casi la mitad de todas las muertes violentas.
Nuestro estudio es proponer un modelo que permita explicar y predecir la
ideación suicida a partir de los problemas de salud mental
(estrés-ansiedad-depresión) y la funcionalidad familiar (cohesión, flexibilidad
y cohesión). Método: Nuestro estudio es transversal. La población estuvo
constituida por médicos internos de todo el Perú. Se utilizó un muestreo no
probabilístico. Se utilizó la Escala de Evaluación de la Cohesión y
Adaptabilidad Familiar (FACES-III), la Escala de Comunicación Familiar, la
Escala de Satisfacción Familiar, Escala de Depresión, Ansiedad y Estrés
(DASS-21) y la Escala de Ideación Suicida - Peor (SSI-W). Resultados: Se
incluyó a un total de 480 participantes. La prevalencia de ideación suicida fue
del 39%. El análisis de regresión de Poisson ajustado identificó que las
personas con síntomas de ansiedad tenían más de cuatro veces más probabilidades
de tener ideación suicida (PR=4.89; IC95%:1.90-12.64). Asimismo, las personas
con niveles de comunicación familiar de moderados a altos eran mucho menos
propensas a tener ideación suicida (PR=0.07; IC95%: 0.01-0.41), lo que lo
convierte en un factor protector. El modelo propuesto presentó óptimos índices
de bondad de ajuste (CFI=0.974; TLI=0.974; SRMR=0.055; RMSEA=0.062). Además, el
modelo propuesto puede explicar la presencia de ideación suicida en un 88,3% (R2=0.883).
Conclusiones: Nuestro modelo puede explicar una gran proporción de las
conductas suicidas basadas en las relaciones familiares y los problemas de
salud mental en médicos internos. Además, las variables que por sí solas se
asociaron más con la conducta suicida fueron los síntomas ansiosos y la
comunicación familiar como factores de riesgo y de protección, respectivamente.
Palabras clave: ideación suicida, depresión, ansiedad, familia,
estrés.
BACKGROUND
As of January 2023, more than 661 million people with
a confirmed diagnosis of COVID-19 and more than 6 million deaths have been
reported to the World Health Organization (WHO) (World Health Organization,
2023). The context of the pandemic has led to the redeployment of health
personnel and materials to focus on COVID-19 areas, the overload of care, the
high risk that health personnel has of becoming
infected with this virus, the shortage of adequate personal protective
equipment, long working hours, and the fear of infecting their families have
all affected the physical and mental health of health personnel (Della Monica
et al., 2022; Huarcaya-Victoria, 2020). A
particularly at-risk group is medical internship students who were exposed to
the clinical context but are more prone to mental health problems because of
their student status (Jacob et al., 2020).
Worldwide, suicides comprise 50% and 71% of reported
violent deaths for males and females, respectively (World Health Organization,
2014). In 2019, the WHO found that each year, approximately 800,000 people
commit suicide, and countless more attempt suicide (World Health Organization,
2021). In 2017, it was the second leading cause of death among university
students (Santos et al., 2017). In some countries, reported suicides are
highest among young people, ranking second worldwide as the leading cause of death
among 15-29-year-olds in 2019
(World Health Organization, 2021). In particular, in Peru,
between 2017 to 2021, the highest incidence of suicide was among people aged 20
to 29 years old (26.2%) and was more frequent in men (69.5%) (Contreras-Cordova
et al., 2022). In addition, between 2004 and 2013, the suicide rate in Peru
increased from 0.46 (CI95%: 0.38-0.55) to 1.13 (CI95%: 1.01-1.25) per 100,000
inhabitants in those years, respectively (Hernández-Vásquez et al., 2016).
One of the many mental health problems today, and
considered one of the most severe because of its likely impact on people’s
lives, is suicidal behavior, which is a largely preventable public health
problem, accounting for almost half of all violent deaths. Suicidal behaviors
present three main clinical manifestations: suicidal ideation, attempted
suicide, and completed suicide (Denis-Rodríguez et al., 2017). Suicidal
ideation is the first of the suicidal behaviors to appear and is one of the
most significant risk signs for suicide prevention (Denis-Rodríguez et al.,
2017). The causation of suicidal ideation is multifactorial. Several studies
have concluded that negative life and mental health events such as
hopelessness, depressive symptomatology, stress, and anxiety are the most common
causes of suicidal ideation (Mortier et al., 2018). Also, social factors such
as those related to family conflicts, academia, and economic factors (Perales
et al., 2019), are the most important predictors for triggering this thinking
type in young university students.
Two main groups of theoretical models attempt to
explain suicidal ideation. On the one hand, those who consider suicidal
ideation to be an individual entity, see it as a clinical manifestation of a
major depressive disorder (American Psychiatric Association, 2013). On the
other hand, trans-diagnostic models consider its origin as part of a continuum
of emotional distress that can develop into mental health problems
(stress-anxiety-depression) (González Pando et al., 2018), Thus, emotionally charged
events such as a pandemic may trigger onset of suicidal ideation. However, both
types of theoretical models consider that social factors and family support
networks play a considerable role in the emergence of these mental health
disorders.
One of the theoretical models that explain family
relationships is Olson’s circumplex model of couple and family systems (Olson
et al., 2019). The circumplex model proposes three dimensions. First, family
cohesion is the relationship between family members. Second, family flexibility
is the ability of the family system to adapt to change and establish norms. In
addition, both dimensions are curvilinear, meaning that very high or low levels
are dysfunctional, and the medium level is functional (Olson et al., 2019).
Third, family communication is the ability of the family system to transmit
information, feelings, and needs between members (Olson et al., 2019). Also, a
facilitating dimension influences the others dimensions. These three variables
together comprise family functionality.
Our study seeks to link both theoretical models
(trans-diagnostic model and circumplex model of the couple and family systems)
to predict the occurrence of suicidal ideation in Peruvian medical students.
Therefore, the general aim of the study is to propose a model that can explain
and predict suicidal ideation based on mental health problems
(stress-anxiety-depression) and family functionality (cohesion, flexibility,
and cohesion).
METHODS
Study design
Our study is cross-sectional.
Setting
During data collection, Peru was facing the third
wave. Although mortality was not as high as in the previous two waves, there
was a rapid increase in the number of confirmed cases due to the new variant
known as omicron, which was more contagious but less lethal. The increase in
confirmed cases generated fear and concern among health personnel, including
medical students, who were no strangers to infection.
Participants
The population consisted of medical students from all
over Peru. The inclusion criteria were that they were over 18 years of age,
agreed to participate in the virtual questionnaire by giving their informed
consent, and were doing their internship in a health center. We excluded
participants who reported receiving antidepressant treatment, those with a
disorder diagnosis, and those who did not complete the questionnaire.
Non-probability sampling was used. A minimum sample
size of 400 participants was calculated since simulation studies have
identified that with at least 400 participants, there would be no significant
changes in the goodness-of-fit indices in the models evaluated when using
structural equation modeling (Iacobucci, 2010).
Variables and instruments
Mental health problems
The DASS-21 has twenty-one Likert-type items with four
response options (0-3 points) and evaluates the symptomatology that
participants have perceived in the last week. The DASS-21 has three dimensions,
the depressive symptoms dimension (items 3, 5, 10, 13, 16, 17, and 21), anxious
symptoms (items 2, 4, 7, 9, 15, 19, and 20), and stress (items 1, 6, 8, 11, 12,
14 and 18) (Lovibond & Lovibond, 1995). A previous study reported optimal
internal consistency values for depressive symptoms (α=0.85), anxious symptoms
(α=0.72), and stress (α=0.79) (Román Mella et al.,
2014). Our prevalence assessment study dichotomized scores for depressive
symptoms (≥14), anxious symptoms (≥10), and stress (≥19) (Lovibond &
Lovibond, 1995).
Family functionality
Family cohesion and adaptability: The Family Cohesion
and Adaptability Evaluation Scale (FACES-III) was applied, with 20 items, with
5-choice Likert-type responses, the odd items are adaptability items, and the
even items are cohesion items (Olson, 1986). The FACES-II has shown evidence of
validity and reliability in Peruvian youth (Bazo-Alvarez
et al., 2016). Our study dichotomized cohesion and adaptability scores. We
considered functionality values for cohesion in the 35 to 45 score range
(separate-connected) and functionality values for adaptability in the 20 to 28
score range (structured-flexible) (Olson, 1986).
Family communication: The Family Communication Scale
(FCS), with 10 Likert-type items with five response options ranging from
strongly disagree to strongly agree (Olson et al., 2019). The FCS has evidence
of validity and reliability (ω>0.80) in the Peruvian context and shows
evidence of factorial independence between men and women (Copez-Lonzoy
et al., 2016). Family communication was considered a linear variable, so scores
≥36 were dichotomized as medium-high (Valle & Cabrera, 2020).
Family satisfaction: The Family Satisfaction Scale
(FSS) consists of ten Likert-type items with five response options ranging from
extremely dissatisfied to extremely satisfied (Olson et al., 2019). In the
Peruvian context, the FSS has evidence of internal structure validity, internal
consistency (ω= 0.925), and gender invariance (Villarreal-Zegarra et al.,
2017). Family satisfaction was considered a linear variable, so scores ≥36 were
dichotomized as medium-high (Valle & Cabrera, 2020).
Suicidal ideation
The Scale for Suicide Ideation – Worst (SSI-W) is a
19-item instrument, with each item having three response options (0 to 2
points), which suggest an increasing level of risk, seriousness, and intensity
of suicidal behavior (Beck et al., 1979). BIS has optimal reliability values in
the overall dimension (α=0.79) (Eugenio Torres & Zelada
Alcántara, 2011) and has been used in studies in the
Peruvian context (Chavez-Cáceres et al., 2020). We
dichotomized the presence of suicidal ideation based on scores ≥14 (Beck et
al., 1999).
Covariates
Our study collects socio-demographic information on
gender (male and female), age group, and with whom they live (live alone or
with at least one family member).
Procedures
The survey link was disseminated through e-mails and
social networks at the national level with the help of the delegates of the
different universities with medical degrees. The time given for its resolution
was two weeks, from 5 to 19 November 2021.
Statistical methods
Correlation analysis
Spearman’s correlation coefficient between variables
was used since it does not require a normal distribution. Cut-offs were
proposed for small (rs > 0.20),
moderate (rs > 0.50), and large (rs > 0.80) effects (Ferguson,
2009).
Regression analysis
We assessed the association of the outcome (suicidal ideation)
with exposure, such as the sociodemographic variables, mental health problems
(anxiety, stress, and depression), and family functionality (family cohesion,
flexibility, and communication). The crude and adjusted prevalence ratio (PR)
was used as a measure of association. The analyses were estimated using
generalized linear models with robust variance estimates, assuming a Poisson
distribution with log link functions (Beran & Violato, 2010).
Structural equation modeling (SEM)
SEM was used with the outcome and exposure variables.
We used the weighted least square mean and variance adjusted (WLSMV) estimator
(Suh, 2015). Also, we used the polychoric correlation matrix (Dominguez-Lara,
2014). The SEM was evaluated in two steps. First, evaluated different
goodness-of-fit indices: Root Mean Squared Error of Approximation (RMSEA),
standardized root mean square (SRMR), comparative fit index (CFI), and Tucker
Lewis index (TLI). The cut-off points of CFI and TLI>0.95; and RMSEA and
SRMR <0.08 were considered (Xia & Yang, 2018). The second step was to
assess the amount of variance explained by perceived stress (output variables)
by the coefficient of determination (R2).
The analyses were performed R Studio, with the
packages “lavaan”, “semTools”,
and “semPlot”.
Ethical aspects
The study
protocol was approved by the ethics committee of the Universidad César Vallejo.
In addition, the ethical norms established in the Declaration of Helsinki were
respected and the participants were asked to sign a virtual informed consent
form.
RESULTS
Participants
A total of 501 Peruvian medical inmates were
evaluated, of whom 480 met the inclusion criteria and were included in the
study. Within the group of excluded inmates, it was identified that they
self-reported having a diagnosis of a mental health problem (n=15), were taking
antidepressants (n=2), or did not agree to participate in the study (n=4).
Among the participants included in the study, the
majority were male (56.7%; n=272), the most frequent age group was between 18
and 25 years old (79.8%; n=383), and the majority lived with at least one
family member (64.0%; n=307). The prevalence of suicidal ideation was estimated
at 39% (n=187). In addition, table 1 shows the prevalence of mental health
problems.
Table 1. Socio-demographic characteristics of participants
(n=480).
|
|
|
n |
% |
|
Sex |
Men |
272 |
56.7% |
|
|
Women |
208 |
43.3% |
|
Age
group |
18 to 25 |
383 |
79.8% |
|
|
26 to 30
|
45 |
9.4% |
|
|
31 to 35
|
21 |
4.4% |
|
|
36 to
more |
27 |
5.6% |
|
|
No
report |
4 |
0.8% |
|
Live
with… |
Lives
with at least one member of your family |
307 |
64.0% |
|
|
Lives
alone |
173 |
36.0% |
|
Depression |
No |
293 |
61.0% |
|
|
Yes |
187 |
39.0% |
|
Anxiety |
No |
282 |
58.8% |
|
|
Yes |
198 |
41.3% |
|
Stress |
No |
365 |
76.0% |
|
|
Yes |
115 |
24.0% |
|
Family
cohesion |
Dysfunctionality |
338 |
70.4% |
|
|
Functionality |
142 |
29.6% |
|
Family
adaptability |
Dysfunctionality |
382 |
79.6% |
|
|
Functionality |
98 |
20.4% |
|
Family
satisfaction |
Low |
277 |
57.7% |
|
|
Medium-High |
203 |
42.3% |
|
Family
communication |
Low |
268 |
55.8% |
|
|
Medium-High |
212 |
44.2% |
|
Suicidal
ideation |
No |
293 |
61.0% |
|
|
Yes |
187 |
39.0% |
Correlation analysis
Our study found a moderate relationship between family
functioning variables and mental health problems (rs>0.70).
In addition, our study found that both family functioning and mental health
problems variables correlated moderately strongly with suicidal ideation in
medical students (rs>0.70).
Table 2 shows the correlation between the mental health problems variables and
the correlation between the family functioning variables.
Table 2. Correlation coefficients between variables of interest
(n=480).
|
|
(1) |
(2) |
(3) |
(4) |
(5) |
(6) |
(7) |
(8) |
|
1.
Depressive symptoms |
1 |
|
|
|
|
|
|
|
|
2.
Anxious symptoms |
0.956 |
1 |
|
|
|
|
|
|
|
3.
Stress |
0.966 |
0.962 |
1 |
|
|
|
|
|
|
4.
Family cohesion |
-0.748 |
-0.757 |
-0.764 |
1 |
|
|
|
|
|
5.
Family adaptability |
-0.729 |
-0.726 |
-0.753 |
0.962 |
1 |
|
|
|
|
6.
Family satisfaction |
-0.755 |
-0.761 |
-0.759 |
0.822 |
0.784 |
1 |
|
|
|
7.
Family communication |
-0.766 |
-0.765 |
-0.769 |
0.819 |
0.786 |
0.916 |
1 |
|
|
8.
Suicidal ideation |
0.742 |
0.743 |
0.748 |
-0.747 |
-0.742 |
-0.738 |
-0.754 |
1 |
Note: All values reported significant values
(p<0.001).
Regression analysis
Poisson regression analysis identified that people
with anxiety symptoms were more than four times more likely to have suicidal
ideation (PR=4.89; 95% CI:1.90 - 12.64). On the other hand, people with
moderate to high levels of family communication were much less likely to have
suicidal ideation (PR= 0.07; 95% CI: 0.01 - 0.41), making it a protective
factor (see Table 3).
Table 3. Raw and adjusted prevalence ratio (PR) for suicidal ideation
(n=480).
|
|
|
rPR |
p |
aPR |
p |
|
Sex |
Men |
1 |
|
1 |
|
|
|
Women |
0.96
[0.72 - 1.28] |
0.764 |
0.97
[0.73 - 1.31] |
0.862 |
|
Live
with… |
Lives
with at least one member of your family |
1 |
|
1 |
|
|
|
Lives
alone |
3.25
[2.41 - 4.39] |
0.000 |
1.18
[0.82 - 1.71] |
0.374 |
|
Depression |
No |
1 |
|
1 |
|
|
|
Yes |
13.08
[8.23 - 20.80] |
0.000 |
0.95
[0.42 - 2.18] |
0.908 |
|
Anxiety |
No |
1 |
|
1 |
|
|
|
Yes |
19.06
[10.85 - 33.49] |
0.000 |
4.89 [1.90 - 12.64] |
0.001 |
|
Stress |
No |
1 |
|
1 |
|
|
|
Yes |
4.74
[3.54 - 6.35] |
0.000 |
1.31
[0.84 - 2.04] |
0.234 |
|
Family cohesion |
Dysfunctionality |
1 |
|
1 |
|
|
|
Functionality |
0.07
[0.03 - 0.16] |
0.000 |
0.77
[0.27 - 2.19] |
0.622 |
|
Family
adaptability |
Dysfunctionality |
1 |
|
1 |
|
|
|
Functionality |
1.35
[0.97 - 1.87] |
0.076 |
1.36
[0.87 - 2.13] |
0.180 |
|
Family
satisfaction |
Low |
1 |
|
1 |
|
|
|
Medium-High |
0.03
[0.01 - 0.08] |
0.000 |
0.97
[0.24 - 3.96] |
0.967 |
|
Family
communication |
Low |
1 |
|
1 |
|
|
|
Medium-High |
0.03
[0.01 - 0.08] |
0.000 |
0.07 [0.01 - 0.41] |
0.003 |
Note: rPR = raw prevalence
ratio. aPR = adjusted prevalence ratio. Model
adjusted by sex, live with other people, depression, anxiety, stress, family
cohesion, family adaptability, family communication, and family satisfaction.
The outcome was suicidal ideation. Values in bold were significant (p<0.05).
Structural equation modeling
Our study presented a model that predicts suicidal
ideation based on family functionality and mental health problems. Our model
proposes that family functioning influences mental health problems because we
found a moderate relationship between the two variables. The proposed model
(see Figure 1) presented optimal goodness-of-fit indices (X2=7364.1;
df=3070; CFI=0.974; TLI=0.974; SRMR=0.055;
RMSEA [90% CI]= 0.062 [0.060 - 0.064]). In addition,
the proposed model can explain the presence of suicidal ideation in 88.3% (R2=0.883).
Our model finds a negative influence of family
functioning on the presence of mental health problems (β=-0.716). In other
words, the higher the family functioning score, the lower the scores for mental
health problems. Furthermore, family functioning has the most influence on the
presence of suicidal ideation (β=-0.561) than mental health problems (β=0.453).
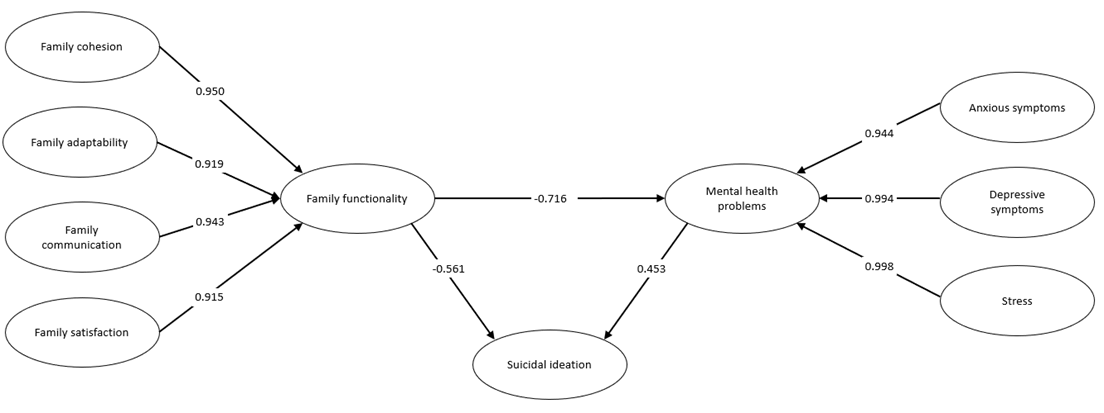
Figure 1. SEM of suicidal ideation, family functionality, and
mental health problems (n=480).
Note: All variables presented are latent, observable
variables (items) are not shown.
DISCUSSION
Main finding and interpretation
Our conclusions propose that the dimensions of the
circumplex model and the mental health problems largely explain suicidal
ideation. Mainly, the most important predictors of suicidal ideation in medical
students are family communication and anxious symptoms. Our study proposes that
family relationships have the most influence on the presence of suicidal
ideation than mental health problems themselves. Based on the circumplex model
theory, balanced families have more functional members with higher well-being
(i.e., less suicidal ideation) than unbalanced families (i.e., low
communication and family satisfaction) (Olson et al., 2019). Therefore, our
study supports this hypothesis of the circumplex model.
Our model also highlights the role of family
relationships in the presence of mental health problems. Therefore, it is of
utmost importance to be able to include family variables in epidemiological
models of mental health problems.
Comparison with other studies
We found other studies that propose explanatory models
using a different variable set. However, they manage to explain a smaller
proportion of suicidal ideation. One study assessed possible mediated variables
for suicidal risk in college students. The study found that impulsivity, family
history of mental disorder and suicide attempt, and history of suicide attempts
in the past year were mediators of suicidal risk (Gómez Tabares
et al., 2019). However, their model only explained 62.7% of suicidal risk.
Another study on adolescents found that family violence and support influence
depressive symptoms and suicidal behavior with peers, and this in turn
influences suicidal ideation (Ramírez & Oduber, 2015). However, the model
is only able to explain 39% of suicidal ideation. Another study on Chinese
university students includes variables such as bullying, internet addiction,
and childhood trauma to explain suicidal ideation (Lu et al., 2020). While this
study achieves adequate goodness-of-fit indices, it does not report how much
the model can explain suicidal ideation. There is heterogeneity in the
variables and methodologies used to propose models to explain suicidal ideation
in medical students. However, we have not found a model that manages to explain
suicidal ideation in such a high percentage as the model we propose.
Systematic reviews and meta-analyses have found
several factors associated with suicidal ideation, such as being female,
alcohol use, having depression, being a junior or pre-clinical student,
exposure to COVID-19, academic stress, history of psychiatric or physical disorders,
financial problems, fear of educational deterioration, online learning
problems, fear of infection, loneliness, low physical activity, low social
support, problematic internet or smartphone use, and young age (Kaggwa et al.,
2023; Peng et al., 2023). In contrast to these findings, our study found that
when adjusting for different variables, anxious symptoms and family
communication are the main risks and protective factors, respectively. Our
results could be explained by the fact that the ability to communicate one’s
emotions and needs within the family could be a protective factor for a college
student to have suicidal thoughts.
As for the prevalence of suicidal ideation,
meta-analyses place it well below the findings of our study. The meta-analyses
report it at 18.7% (95% CI: 14.1%-23.3) (Kaggwa et al., 2023), 15 % (95 % CI,
11 %-18 %) (Peng et al., 2023), and 11.1% (95% CI, 9.0% to 13.7%) (Rotenstein et al., 2016).
Therefore, the sample assessed may have a high prevalence of suicidal
ideation compared to that reported by other studies. One possible explanation
for the potential increase in suicidal ideation is the context of COVID-19,
which generated an increase in the prevalence of mental health problems (Meda et al., 2021).
Public health implications
The findings of our study could be used to guide the
formulation of policies and programs to address suicidal behavior in medical
students. Interventions could be implemented to improve family communication
and address anxiety symptoms in medical students, to reduce mental health
problems (Fulgoni et al., 2019). In addition, the high level of suicidal
ideation found in medical students suggests the need for preventive
interventions to address this public health problem. This could include
workplace suicide prevention programs and emotional support programs for
medical students (Joshi et al., 2015; Skaczkowski et
al., 2022; Witt et al., 2019).
Limitations and strengths
We have identified three limitations in our study.
First, our study is cross-sectional. Therefore, causal relationships should not
be assumed. Secondly, our study may have errors in the measurement of outcome
or exposure factors. Although we use validated psychometric instruments, this
is not a substitute for a gold standard such as a clinical interview with a
mental health professional. Third, our study is not probabilistic. Four, other
variables that could potentially better explain suicidal ideation, such as
family violence, history of suicide attempts, or self-harming behavior, were
not included. Fourth, it was not possible to perform a mediation or moderation
analysis because the assumptions of the analysis were not met. Therefore, the
results are not representative of all medical interns in Peru. On the other
hand, the main strength of our study is that it includes many variables to
explain the full spectrum of family relationships and the most frequent mental
health problems.
Conclusions
Our model can explain 88.3% of suicidal behavior based
on family relationships and mental health problems in medical interns. In
addition, the variables that alone were most associated with suicidal behavior
were anxious symptoms and family communication as risk factors and protective
factors, respectively. Also, we found a high prevalence of suicidal ideation
(39%) in medical interns. Our study suggests that family relationships
influence suicidal ideation, so interventions based on improving family
relationships could reduce suicidal ideation in Peruvian medical interns.
ORCID
Leslie Aguilar-Sigueñas https://orcid.org/0000-0002-6677-5904
David Villarreal-Zegarra https://orcid.org/0000-0002-2222-4764
CONTRIBUTION OF THE AUTHORS
Leslie Aguilar-Sigueñas:
Conceptualization, Formal analysis, Investigation, Data Curation, Writing -
Original Draft, Visualization.
David Villarreal-Zegarra: Conceptualization,
Methodology, Software, Formal analysis, Writing - Review & Editing,
Supervision.
FUNDING
Our study was self-funded.
CONFLICTS OF INTEREST
DVZ is editor of Interacciones.
The study is part of an LAS graduate thesis.
ACKNOWLEDGMENTS
None.
REVIEW PROCESS
This study has been reviewed by external peers in a
double-blind mode. The editor in charge Renzo Rivera.
The review process can be found as supplementary material 1.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are
openly available in supplementary material 2.
DISCLAIMER
The authors are responsible for all statements made in
this article.
REFERENCES
American Psychiatric Association (2013). Guía de consulta de los criterios
diagnósticos del DSM 5. Asociación Americana de Psiquiatría; Arlington, VA.
Bazo-Alvarez, J. C., Bazo-Alvarez, O. A., Aguila, J.,
Peralta, F., Mormontoy, W., & Bennett, I. M.
(2016). Propiedades psicométricas de la escala de funcionalidad familiar
FACES-III: un estudio en adolescentes peruanos. Revista peruana de medicina
experimental y salud publica, 33(3),
462–470. https://doi.org/10.17843/rpmesp.2016.333.2299
Beck, A. T., Brown, G. K., Steer, R. A., Dahlsgaard, K. K., & Grisham, J. R. (1999). Suicide
ideation at its worst point: a predictor of eventual suicide in psychiatric
outpatients. Suicide & Life-Threatening Behavior, 29(1), 1–9.
https://www.ncbi.nlm.nih.gov/pubmed/10322616
Beck, A. T., Kovacs, M., & Weissman, A. (1979).
Assessment of suicidal intention: the Scale for Suicide Ideation. Journal of
Consulting and Clinical Psychology, 47(2), 343–352.
https://doi.org/10.1037//0022-006x.47.2.343
Beran, T. N.,
& Violato, C. (2010). Structural equation modeling in medical research: a
primer. BMC Research Notes, 3, 267.
https://doi.org/10.1186/1756-0500-3-267
Chavez-Cáceres, R.,
Luna-Muñoz, C., Mendoza-Cernaqué, S., Ubillus, J. J., & Lopez, L. C. (2020). Factors
associated with suicide ideation in patients of a Peruvian Hospital. Revista de la Facultad de Medicina Humana, 20(3), 1–1. https://doi.org/10.25176/RFMH.v20i3.3054
Contreras-Cordova, C. R., Atencio-Paulino, J. I., Sedano, C., Ccoicca-Hinojosa,
F. J., & Huaman, W. P. (2022). Suicidios en el
Perú: Descripción epidemiológica a través del Sistema Informático Nacional de
Defunciones (SINADEF) en el periodo 2017-2021. Revista de neuro-psiquiatria, 85(1), 19–28.
https://doi.org/10.20453/rnp.v85i1.4152
Copez-Lonzoy, A. J.
E., Villarreal-Zegarra, D., & Paz-Jesús, Á. (2016). Propiedades
psicométricas de la Escala de Comunicación Familiar en estudiantes universitarios.
Revista Costarricense de Psicología, 35(1), 31–46.
https://doi.org/10.22544/rcps.v35i01.03
Della Monica, A., Ferrara,
P., Dal Mas, F., Cobianchi,
L., Scannapieco, F., & F Ruta, F. R. (2022). The impact of Covid-19 healthcare emergency on the
psychological well-being of health professionals: a review of literature. Annali Di Igiene: Medicina
Preventiva E Di Comunita, 34(1), 34.
https://doi.org/10.7416/ai.2021.2445
Denis-Rodríguez, E., Alarcón, M. E. B.,
Delgadillo-Castillo, R., Denis-Rodríguez, P. B., & Melo-Santiesteban, G.
(2017). Prevalence of Suicidal Ideation in Medical
Students of Latin America: a Meta-analysis. RIDE Revista Iberoamericana Para La Investigación Y El
Desarrollo Educativo, 8(15), 387–418.
https://doi.org/10.23913/ride.v8i15.304
Dominguez-Lara, S.
(2014). ¿Matrices Policóricas/Tetracóricas
o Matrices Pearson? Un estudio metodológico. Revista Argentina de Ciencias
Del Comportamiento, 6(1), 39–48.
https://doi.org/10.32348/1852.4206.v6.n1.6357
Eugenio Torres, S. R., & Zelada Alcántara, M. B.
(2011). Relación entre estilos de afrontamiento e ideación suicida en
pacientes viviendo con VIH del GAM “Somos Vida” del hospital nacional Sergio E.
Bernales de la ciudad de Lima (M. E. Dorival
Sihuas (ed.)) [Licenciatura en Psicología , Universidad
Señor de Sipán]. https://hdl.handle.net/20.500.12802/1600
Ferguson, C. J. (2009). An effect size primer: A guide
for clinicians and researchers. Professional Psychology: Research and
Practice, 40(5), 532–538. https://doi.org/10.1037/a0015808
Fulgoni, C. M. F., Melvin, G. A., Jorm,
A. F., Lawrence, K. A., & Yap, M. B. H. (2019). The Therapist-assisted
Online Parenting Strategies (TOPS) program for parents of adolescents with
clinical anxiety or depression: Development and feasibility pilot. Internet Interventions, 18, 100285.
https://doi.org/10.1016/j.invent.2019.100285
Gómez Tabares, A. S., Núñez, C., Caballo, V. E.,
Agudelo Osorio, M. P., Aguirre, G., & Mauricio, A. (2019). Predictores
psicológicos del riesgo suicida en estudiantes universitarios. Behavioral Psychology /
Psicología Conductual, 27(3), 391–413.
González Pando, D., Cernuda Martínez, J. A., Alonso
Pérez, F., Beltrán García, P., & Aparicio Basauri, V. (2018). Transdiagnóstico: origen e implicaciones en los cuidados de
salud mental. Revista de La Asociación Española de Neuropsiquiatría, 38(133),
145–166. https://doi.org/10.4321/s0211-57352018000100008
Hernández-Vásquez, A., Azañedo,
D., Rubilar-González, J., Huarez, B., & Grendas, L. (2016). Evolución y diferencias regionales de
la mortalidad por suicidios en el Perú, 2004-2013. Revista Peruana de
Medicina Experimental Y Salud Pública, 33(4), 751–757.
https://doi.org/10.17843/rpmesp.2016.334.2562
Huarcaya-Victoria, J. (2020). Consideraciones sobre la
salud mental en la pandemia de COVID-19. Revista Peruana de Medicina
Experimental Y Salud Pública, 37(2), 327–334.
https://doi.org/10.17843/rpmesp.2020.372.5419
Iacobucci, D. (2010). Structural equations modeling: Fit
Indices, sample size, and advanced topics. Journal of Consumer Psychology,
20(1), 90–98. https://doi.org/10.1016/j.jcps.2009.09.003
Jacob, R., Li, T.-Y., Martin, Z., Burren, A., Watson,
P., Kant, R., Davies, R., & Wood, D. F. (2020). Taking care of our future
doctors: a service evaluation of a medical student mental health service. BMC
Medical Education, 20(1), 1–11.
https://doi.org/10.1186/s12909-020-02075-8
Joshi, S. V., Hartley, S. N., Kessler, M., & Barstead, M. (2015). School-based suicide prevention:
content, process, and the role of trusted adults and peers. Child and
Adolescent Psychiatric Clinics of North America, 24(2), 353–370.
https://doi.org/10.1016/j.chc.2014.12.003
Kaggwa, M. M., Najjuka, S.
M., Favina, A., Griffiths, M. D., & Mamun, M. A.
(2023). Suicidal behaviors and associated factors among medical students in
Africa: A systematic review and meta-analysis. Journal of Affective
Disorders Reports, 11, 100456.
https://doi.org/10.1016/j.jadr.2022.100456
Lovibond, S. H., & Lovibond, P. F. (1995). Manual
for the depression anxiety stress scales. Psychology Foundation of
Australia; Sydney, Australia. https://doi.org/10.1037/t01004-000
Lu, L., Jian, S., Dong, M., Gao, J., Zhang, T., Chen,
X., Zhang, Y., Shen, H., Chen, H., Gai, X., & Liu, S. (2020). Childhood
trauma and suicidal ideation among Chinese university students: the mediating
effect of Internet addiction and school bullying victimisation.
Epidemiology and Psychiatric Sciences, 29, e152.
https://doi.org/10.1017/S2045796020000682
Meda, N., Pardini, S., Slongo,
I., Bodini, L., Zordan, M.
A., Rigobello, P., Visioli,
F., & Novara, C. (2021). Students’ mental health problems before, during,
and after COVID-19 lockdown in Italy. Journal of Psychiatric Research, 134,
69–77. https://doi.org/10.1016/j.jpsychires.2020.12.045
Mortier, P., Auerbach, R. P., Alonso, J., Bantjes, J., Benjet, C., Cuijpers, P., Ebert, D. D., Green, J. G., Hasking, P., Nock, M. K., O’Neill, S., Pinder-Amaker, S., Sampson, N. A., Vilagut,
G., Zaslavsky, A. M., Bruffaerts,
R., Kessler, R. C., & WHO WMH-ICS Collaborators. (2018). Suicidal Thoughts
and Behaviors Among First-Year College Students: Results From the WMH-ICS
Project. Journal of the American Academy of Child and Adolescent Psychiatry,
57(4), 263–273.e1. https://doi.org/10.1016/j.jaac.2018.01.018
Olson, D. H. (1986). Circumplex Model VII: validation
studies and FACES III. Family Process, 25(3), 337–351.
https://doi.org/10.1111/j.1545-5300.1986.00337.x
Olson, D. H., Waldvogel, L.,
& Schlieff, M. (2019). Circumplex Model of
Marital and Family Systems: An Update. Journal of Family Theory & Review,
11(2), 199–211. https://doi.org/10.1111/jftr.12331
Peng, P., Hao, Y., Liu, Y., Chen, S., Wang, Y., Yang,
Q., Wang, X., Li, M., Wang, Y., He, L., Wang, Q., Ma, Y., He, H., Zhou, Y., Wu,
Q., & Liu, T. (2023). The prevalence and risk factors of mental problems in
medical students during COVID-19 pandemic: A systematic review and
meta-analysis. Journal of Affective Disorders, 321, 167–181.
https://doi.org/10.1016/j.jad.2022.10.040
Perales, A., Sánchez, E., Barahona, L., Oliveros, M.,
Bravo, E., Aguilar, W., Ocampo, J. C., Pinto, M., Orellana, I., & Padilla,
A. (2019). Prevalencia y factores asociados a
conducta suicida en estudiantes de la Universidad Nacional Mayor de San Marcos,
Lima-Perú. Anales de La Facultad de Medicina, 80(1), 28–33.
https://doi.org/10.15381/anales.v80i1.15865
Ramírez, J. A. R., & Oduber, J. A. (2015). Ideación suicida y grupo de iguales: análisis en una
muestra de adolescentes venezolanos. Universitas
Psychologica, 14(3).
https://doi.org/10.11144/Javeriana.upsy14-3.isgi
Román Mella, F., Vinet, E. V., & Alarcón Muñoz, A.
M. (2014). Escalas de Depresión, Ansiedad y Estrés (DASS-21): Adaptación y
propiedades psicométricas en estudiantes secundarios de temuco.
Revista Argentina de Clínica Psicológica, 23(2), 179–190.
Rotenstein, L. S.,
Ramos, M. A., Torre, M., Segal, J. B., Peluso, M. J.,
Guille, C., Sen, S., & Mata, D. A. (2016). Prevalence of Depression, Depressive Symptoms, and
Suicidal Ideation Among Medical Students: A Systematic Review and
Meta-Analysis. JAMA: The Journal of the American Medical Association, 316(21),
2214–2236. https://doi.org/10.1001/jama.2016.17324
Santos, H. G. B. dos, dos Santos, H. G. B., Marcon, S. R., Espinosa, M. M., Baptista, M. N., & de
Paulo, P. M. C. (2017). Factors
associated with suicidal ideation among university students. Revista Latino-Americana de Enfermagem,
25, e2878. https://doi.org/10.1590/1518-8345.1592.2878
Skaczkowski, G., van der Kruk, S., Loxton, S., Hughes-Barton, D.,
Howell, C., Turnbull, D., Jensen, N., Smout, M.,
& Gunn, K. (2022). Web-Based Interventions to Help Australian Adults
Address Depression, Anxiety, Suicidal Ideation, and General Mental Well-being:
Scoping Review. JMIR Mental Health, 9(2), e31018.
https://doi.org/10.2196/31018
Suh, Y. (2015). The Performance of Maximum Likelihood
and Weighted Least Square Mean and Variance Adjusted Estimators in Testing
Differential Item Functioning With Nonnormal Trait
Distributions. Structural Equation Modeling: A Multidisciplinary Journal,
22(4), 568–580. https://doi.org/10.1080/10705511.2014.937669
Valle, W., & Cabrera, M. (2020). Valores normativos de las escalas de satisfacción y
comunicación familiar: Un estudio preliminar. Teoría y Práctica: Revista Peruana de Psicología, 1(1), e23.
Villarreal-Zegarra, D., Copez-Lonzoy,
A., Paz-Jesús, A., & Costa-Ball, C. D. (2017). Validez y confiabilidad de
la Escala Satisfacción Familiar en estudiantes universitarios de Lima
Metropolitana, Perú. Actualidades en Psicología, 31(123), 90–99.
https://doi.org/10.15517/ap.v31i123.23573
Witt, K., Boland, A., Lamblin,
M., McGorry, P. D., Veness,
B., Cipriani, A., Hawton, K., Harvey, S.,
Christensen, H., & Robinson, J. (2019). Effectiveness of universal programmes
for the prevention of suicidal ideation, behaviour
and mental ill health in medical students: a systematic review and
meta-analysis. Evidence-Based Mental Health, 22(2), 84–90.
https://doi.org/10.1136/ebmental-2019-300082
World Health Organization. (2014). Preventing
Suicide: a Global Imperative. WHO; Geneva, Geneva.
World Health Organization. (2021). Suicidio.
World Health Organization.
https://www.who.int/es/news-room/fact-sheets/detail/suicide
World Health Organization. (2023). WHO Coronavirus
Disease (COVID-19) Dashboard. World Health Organization.
https://doi.org/10.46945/bpj.10.1.03.01
Xia, Y., & Yang, Y. (2018). RMSEA, CFI, and TLI in
structural equation modeling with ordered categorical data: The story they tell
depends on the estimation methods. Behavior Research Methods, 51(1),
409–428. https://doi.org/10.3758/s13428-018-1055-2